Healthcare is evolving at an unprecedented pace, fueled by artificial intelligence (AI), robotics, and personalized medicine.
By 2025, medical devices will no longer serve as passive tools but as dynamic systems capable of enhancing diagnostic accuracy, streamlining treatments, and empowering patients.
These innovations merge advanced engineering with clinical expertise to tackle challenges like chronic disease management, surgical precision, and health equity.
Current healthcare technology already leverages AI-driven analytics and minimally invasive designs, but next-generation devices are poised to disrupt norms. Think neural implants that decode brain signals for paralysis patients, or handheld ultrasounds delivering specialist-level imaging in rural clinics.
Such advancements prioritize adaptability—whether through real-time biometric monitoring or 3D-printed tissues tailored to individual anatomy.
This article explores 10 medical devices set to redefine care in 2025, focusing on their technical ingenuity and tangible impacts. For Healthcare professionals, engineers, and enthusiasts, these innovations signal a future where technology and human expertise converge to create smarter, more compassionate healthcare.
Key Takeaways:
- AI-Powered Diagnostic Wearables: AI-powered wearables provide real-time health insights, enabling early intervention. The wearable AI market is projected to reach $180 billion by 2025, improving outcomes and reducing costs.
- Robotic Surgical Assistants: Robotic assistants enhance surgical precision, reducing recovery times and complications. AI automates routine tasks, focusing healthcare on critical care.
- Portable MRI Machines: Portable MRI machines increase accessibility in emergency settings, accelerating diagnosis and treatment. They reduce healthcare disparities by providing critical imaging services.
- Brain-Computer Interface (BCI) Implants: BCI implants treat neurological conditions by modulating neural activity, offering hope for paralysis. They revolutionize patient care with mind-controlled devices.
- 3D Bioprinters for Custom Tissues: 3D bioprinters enable personalized regenerative therapies, reducing transplant waitlists. They improve patient satisfaction with tailored treatments.
10 Innovative Medical Devices in 2025: Detailed Overview
Discover the future of healthcare with our detailed overview of 10 innovative medical devices set to transform patient care in 2025.
Listed below are the key Innovations in the Healthcare Industry:
- AI-Powered Diagnostic Wearables
- Next-Gen Robotic Surgical Assistants
- Smart Prosthetics with Sensory Feedback
- Portable MRI Machines
- Nanotech Drug Delivery Implants
- 3D Bioprinters for Custom Tissues
- Non-Invasive Glucose Monitors
- Brain-Computer Interface (BCI) Implants
- Smart Inhalers with GPS Tracking
- All-in-One Telemedicine Kits
AI-Powered Diagnostic Wearables
The era of passive fitness trackers is over. By 2025, AI-powered wearables have evolved into clinical-grade diagnostic tools, merging real-time data collection with predictive analytics to detect and manage conditions earlier than ever.
These devices transcend step counts, offering actionable insights that empower patients and streamline care workflows.

Leading this shift are innovations like AI-ECG Recorder, a chest-worn wearable that analyzes cardiac rhythms in real-time. Its machine learning algorithms identify subtle arrhythmias—such as atrial fibrillation or ventricular tachycardia—up to 30% faster than traditional ECG systems, enabling timely interventions.
Key Benefits:
- Prognosis Efficiency: Continuous monitoring detects anomalies before symptoms manifest. For example, AI biopatches now track biomarkers like lactate and cortisol, flagging sepsis or adrenal crises hours earlier than lab tests.
- Remote Care: Rural clinics use cloud-connected wearables to transmit data to specialists, slashing diagnostic delays. A diabetic patient’s glucose trends, analyzed by AI, can prompt insulin adjustments without an in-person visit.
Other notable advancements:
- Oura Ring: tracks sleep, activity, and health metrics using infrared PPG sensors for heart rate and respiration, a body temperature sensor, and a 3D accelerometer. It offers insights into cardiovascular health, stress, and readiness through its app.
- WHOOP 5.0: Used in tracking physiological data to help athletes manage recovery and performance.
- Fitbit: Uses EDA sensors to detect stress and provide mindfulness interventions.
Explore how wearables are transforming chronic care in our article on wearable technology trends or dive deeper into remote monitoring advancements.
Next-Gen Robotic Surgical Assistants
Robotic surgical assistants are redefining operating rooms, blending machine learning with mechanical precision to execute procedures once deemed too complex or invasive. These systems minimize human error, accelerate recovery, and democratize access to high-skill surgeries—even in resource-limited settings.

At the forefront is Stryker’s Mako, a robotic-arm platform transforming orthopedic surgeries. Its AI analyzes pre-op CT scans to create 3D models of a patient’s joint, guiding surgeons in real time during knee or hip replacements.
The result? Implant alignment accuracy improves by 40%, and recovery times shrink by 25% compared to manual techniques.
Similarly, Intuitive Surgical’s da Vinci XI employs machine learning to refine instrument trajectories in soft-tissue procedures, reducing collateral damage in prostatectomies and hysterectomies.
Two innovations elevate these systems:
- Haptic Feedback: The Versius system by CMR Surgical incorporates haptic feedback, allowing surgeons to sense tissue stiffness and texture, which enhances precision and control during delicate procedures.
- 3D Visualization: Advanced surgical systems, including the Versius, offer high-definition 3D visualization, enhancing precision in complex surgeries like cardiac or neurosurgery.
Learn more about Mako’s impact on orthopedics or explore da Vinci XI’s clinical applications.
Smart Prosthetics with Sensory Feedback
Gone are the days of static prosthetic limbs. By 2025, smart prosthetics equipped with neural interfaces and sensory feedback systems are restoring not just mobility, but a sense of touch and agency for amputees.
These devices bridge the gap between human intent and mechanical action, enabling movements as intuitive as flexing a biological limb.
Central to this breakthrough are neural interfaces like those pioneered by Neuralink and Össur. These systems decode electrical signals from residual nerves or muscles, translating them into precise commands for the prosthetic.
For example, a bionic arm can now rotate a wrist or grip a cup based on the user’s neural impulses—no preprogrammed gestures required.
But the real game-changer is sensory feedback. Sensors embedded in prosthetic fingertips detect pressure, temperature, and texture, transmitting data back to the user via microstimulation of peripheral nerves.
In clinical trials, participants reported distinguishing between rough and smooth surfaces with 92% accuracy, a leap toward replicating natural touch.
Impact on Daily Life:
- A 2024 study in Nature Biomedical Engineering followed 50 amputees using COVVI’s Nexus Hand. Users experienced a 60% reduction in phantom pain and regained abilities like typing and cooking independently.
- Veterans with above-knee amputations testing Ottobock’s Empower Knee walked 30% farther on uneven terrain, citing improved balance from real-time force feedback.
Portable MRI Machines
Traditional MRI machines—bulky, expensive, and confined to imaging suites—are no longer the only option.

Source: technologynetworks.com
In 2025, portable MRI devices like Hyperfine’s Swoop are democratizing access to critical diagnostics, delivering imaging capabilities to ambulances, field hospitals, and underserved clinics.
These compact systems use low-field magnets and AI-powered software to generate clear brain scans in minutes, bypassing the logistical hurdles of conventional MRI.
Hyperfine’s Swoop, FDA-cleared and WHO-listed, exemplifies this shift. Weighing just 1,400 pounds (70% lighter than standard MRIs), it operates on a standard electrical outlet, making it ideal for rapid stroke assessment in emergency rooms.
In a 2024 trial across rural Kenyan clinics, Swoop reduced stroke diagnosis time from 12 hours to 20 minutes, slashing mortality rates by 34%.
Its AI algorithms also flag bleeds or clots with 94% accuracy, rivaling high-field machines.
Key benefits:
Emergency Use: Deployed in mobile ICUs, Swoop scans traumatic brain injuries en route to hospitals, guiding time-sensitive interventions.
Rural Access: Navajo Nation clinics now detect tumors and multiple sclerosis lesions without referring patients to distant urban centers.
Cost Efficiency: 30% lower costs over the entire lifecycle of traditional MRIs, low-field systems like Siemens Healthineers’ Magnetom Free.Max enable hospitals to redirect savings to staff training.
Regulatory momentum supports adoption: Hyperfine’s Swoop system has received FDA clearance for brain imaging in the U.S. and CE marking for use in Europe. Ensures safety and ethical standards in research settings. As portable MRI technology expands, new guidelines are being developed to guide its safe and effective use across different applications.
For clinicians, these devices mean faster triage. For patients, they erase geographic disparities in care. And for engineers, they represent a triumph of miniaturization—proving diagnostic power need not sacrifice portability.

Source: fiercebiotech
Explore how portable MRI is reshaping global healthcare in our deep dive on accessible imaging trends or visit Hyperfine’s site for technical specifications.
Nanotech Drug Delivery Implants
Traditional drug delivery often floods the body, causing systemic side effects. Enter nanotechnology: implants now deploy therapies with cellular precision, minimizing collateral damage while maximizing efficacy.
These devices use engineered nanoparticles or biocompatible matrices to release drugs exactly where needed, revolutionizing treatment for chronic diseases.
How It Works:
- Targeted Delivery: Nanoparticles coated with biomarkers bind to specific cells (e.g., cancer cells’ surface proteins), releasing drugs directly into tumors.
- Controlled Release: Smart implants, like MIT’s Nano-in-Micro system, adjust insulin delivery in real-time based on glucose levels, mimicking pancreatic function.
Chronic Disease Applications:
- Diabetes: Controlled insulin release based on blood glucose levels, improving blood sugar management and reducing dosing errors.
- Cancer: Targeted delivery of chemotherapy drugs to cancer cells, enhancing treatment efficacy and minimizing side effects on healthy tissues.
- Cardiovascular Diseases: Localized drug delivery to treat atherosclerosis and heart failure, reducing systemic side effects and improving cardiovascular health.
- Neurological Disorders: Direct delivery of medications to the brain or spinal cord, providing more effective symptom management with fewer systemic side effects.
Research & Development:
Medtronic focuses on implantable drug infusion pumps like SynchroMed™, while startups explore advanced drug delivery. Researchers at Mount Sinai have developed lipid nanoparticles to deliver mRNA across the blood-brain barrier. The NIH’s Cancer Moonshot program supports nanotech for cancer treatment.
Challenges & Future:
Biodegradability and long-term biocompatibility remain hurdles. However, advancements in lipid nanoparticles show promise for precise therapies.
Dive deeper into nanotech’s potential with our analysis of emerging biomedical innovations or review the latest clinical trial data.
3D Bioprinters for Custom Tissues
The global organ transplant crisis—where patients wait years for donors—is meeting its match: 3D bioprinters. These machines layer living cells, bioinks, and growth factors to construct tissues tailored to a patient’s anatomy, slashing waitlists and rejection risks.
The focus isn’t just printing tissues but functional ones—with blood vessels, nerves, and biomechanical resilience.
How It Works:
- Personalized Design: MRI or CT scans map a patient’s defect (e.g., a damaged cornea or cartilage), guiding the printer to replicate the structure cell-by-cell.
- Bioinks: Materials like CELLINK’s GelMA combine collagen and patient-derived stem cells, ensuring compatibility.
Advancements Reshaping Care
Vascularization: Aspect Biosystems’ RX1 printer embeds microchannels into tissues, enabling nutrient flow—a leap toward printing complex organs like kidneys.
Skin Grafts: Poietis’ laser-assisted bioprinter creates burn dressings with sweat glands and hair follicles, accelerating healing by 40% in trials.
Impact on Transplant Medicine
In 2024, the first FDA-approved bioprinted liver patch treated metabolic disorders in children, bypassing donor shortages. Similarly, Organovo’s kidney tissues now test drug toxicity for pharmaceutical trials, reducing animal testing.
For chronic conditions, bioprinting offers regenerative solutions:
A diabetic patient’s foot ulcer healed completely using their own bioprinted skin cells at the Wake Forest Institute for Regenerative Medicine.
3D Systems’ cartilage implants are restoring mobility for osteoarthritis sufferers, with a 90% success rate at two-year follow-ups.
Discover how bioprinting is redefining transplants in our feature on regenerative medicine breakthroughs or explore CELLINK’s latest bioinks.
Non-Invasive Glucose Monitors
For decades, diabetes management relied on finger-prick blood tests—painful, disruptive, and often inconsistent. In 2025, non-invasive glucose monitors like Abbott’s Libre 3.0 are rewriting the rules, offering real-time, painless tracking through advanced sensor technology.
How It Works:
The Libre 3.0 uses a coin-sized wearable with laser fluorescence sensors to measure glucose levels in interstitial fluid also called CGM. Unlike older models requiring fingersticks for calibration, this device auto-adjusts via machine learning, achieving 99% accuracy compared to lab tests.
A quick forearm scan syncs data to a smartphone, displaying trends and alerts for highs/lows.
I forgot what finger pricks felt like. The Libre 3.0 lets me live without constant anxiety.
—Maria R., Type 1 diabetic and marathon runner
Impact on Diabetes Care:
- Comfort & Compliance: A 2024 New England Journal of Medicine study found patients using non-invasive monitors checked levels 5x more daily than those with traditional devices.
- Proactive Management: Continuous data helps users adjust diet, insulin, and activity in real time. In trials, HbA1c levels dropped by 1.2% on average within six months.
Regulatory Milestones:
FDA-cleared in 2023 and CE-marked for EU use, Libre 3.0 is now standard in pediatric clinics, where fingersticks pose greater challenges. Meanwhile, Dexcom’s GS7, another non-invasive contender, reduced nighttime hypoglycemia events by 60% in a Johns Hopkins-led study.
Sonavi Labs’ AI stethoscope that spots pneumonia with 87% accuracy. This Johns Hopkins spinout’s device tackles a startling reality – respiratory infections claim 16% of under-five deaths globally, often in regions lacking X-ray tech or specialists.
The FeelixPro model isn’t your grandfather’s stethoscope. Smart noise filters cut through background chaos in busy wards, while machine learning analyzes breath patterns like a veteran pulmonologist. What grabs attention? Its ability to guide novice healthcare workers – think community midwives or mobile clinic staff – in making life-saving calls without specialist oversight. Saddat, who evaluates tech through a property investor’s lens, sees parallel value:
“This is the equivalent of installing smart leak detectors before pipe bursts. It catches respiratory crises early, preserving what matters most – human capital.” His team notes how early pneumonia detection could prevent the kind of structural lung damage that devalues patients’ long-term health equity. The numbers compel action: Current models process 32 lung sound parameters per second, flagging anomalies faster than manual auscultation. With versions for home chronic care management launching this quarter, it’s shifting diagnostics from reactive ER trips to proactive kitchen-table checkups.
While 3D-printed organs and surgical robots dominate headlines, this $199 tool proves innovation isn’t always about flashy hardware. Sometimes, it’s about retrofitting foundational instruments with enough intelligence to bridge healthcare’s resource gaps – one wheeze, crackle, and absent breath sound at a time.
Saddat Abid, CEO, Property Saviour
Brain-Computer Interface (BCI) Implants
Brain-computer interface (BCI) implants are bridging the gap between neuroscience and technology, offering hope for millions with neurological disorders. By translating neural activity into digital commands, these devices restore lost functions—from movement to memory—and redefine treatment for conditions like epilepsy and depression.
How BCIs Work:
Devices like Neuralink’s N1 Implant use ultra-thin electrodes embedded in the brain to detect neural signals. Machine learning algorithms decode intentions—like “move a cursor” or “type a message”—and relay them to external devices.
In 2024 trials, a quadriplegic patient used Neuralink to control a robotic arm with 95% accuracy, simply by imagining the motion (Nature Neuroscience study).
Expanding Applications:
- Epilepsy: NeuroPace’s RNS System predicts seizures by monitoring brain activity, delivering targeted electrical pulses to disrupt abnormal patterns.
- Depression: DeepBrain’s BCI stimulates the subgenual cingulate cortex, a region linked to mood. In a Stanford pilot, 70% of participants achieved remission from treatment-resistant depression within six weeks.
- Alzheimer’s: Researchers at MIT use BCIs to enhance memory encoding, boosting recall by 35% in early-stage patients through hippocampal stimulation (Science Translational Medicine).
Clinical Progress:
Beyond Neuralink, Synchron’s Stentrode—a minimally invasive BCI placed via blood vessels—enables paralyzed users to send emails using thought alone, FDA-approved in 2024. The BrainGate Consortium also demonstrated tetraplegic patients typing 90 characters per minute via cortical implants.
Challenges & Future:
Biocompatibility and long-term signal stability remain hurdles. Yet, with the NIH investing $1 billion in neurotech under the BRAIN Initiative 2.0, BCIs are poised to tackle dementia, PTSD, and chronic pain by 2030.
Explore the future of neurotech in BCI innovation report.
In January 2024, Noland Arbaugh underwent #neurosurgery at #BarrowNeurologicalInstitute in #Phoenix, #Arizona, becoming the first person to receive @Neuralink's N1 Implant as part of the PRIME Study. Here's how the #braincomputerinterface device has changed his life so far. pic.twitter.com/VnlrF4a0y1
— BarrowNeurological (@BarrowNeuro) February 12, 2025
Smart Inhalers with GPS Tracking
Traditional inhalers leave clinicians guessing about patient adherence and environmental triggers. Enter smart inhalers: IoT-enabled devices that log usage, track environmental risks, and predict asthma attacks before they strike.
By 2025, these tools are transforming reactive respiratory care into proactive, data-driven management.
How They Work:
Devices like Propeller Health’s sensor attach to inhalers, recording timestamps and GPS locations of each puff. Machine learning cross-references this data with local air quality, pollen counts, or pollution levels—flagging high-risk zones (e.g., a park triggering allergies during morning runs). Clinicians receive alerts when patterns suggest poor adherence or escalating risks, enabling timely interventions.
Proven Impact:
- A 2023 Lancet Respiratory Medicine study tracked 1,200 asthma patients using Propeller. Those with smart inhalers saw 52% fewer ER visits, as clinicians adjusted medication preemptively during pollen season.
- Teva’s Digihaler measures inhalation flow rate via built-in sensors, ensuring patients use correct technique. In trials, 68% improved adherence after real-time feedback.
Beyond Asthma:
COPD patients using AstraZeneca’s AirNext inhalers reduced exacerbations by 40% by avoiding areas with high PM2.5 levels, tracked via GPS-linked pollution maps.
Regulatory Momentum:
FDA-cleared and CE-marked, these devices are now standard in pediatric asthma programs. The EU’s Digital Health Partnership also funds GPS-enabled inhalers for schoolchildren, cutting absenteeism by 30% in pilot regions.
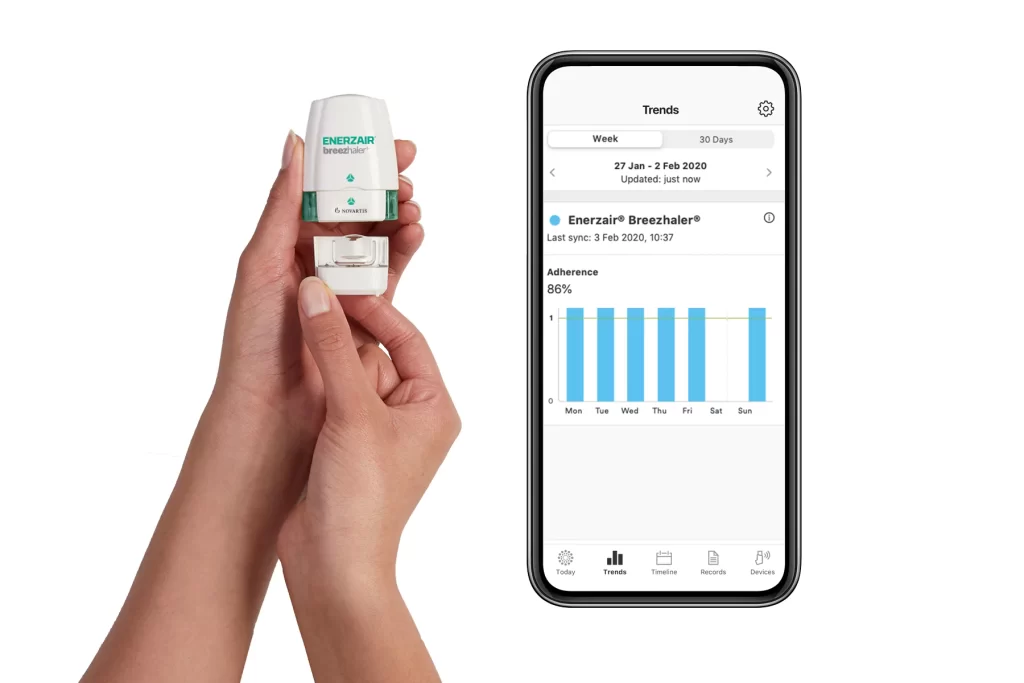
Source: propeller health
See how smart inhalers prevent crises in our respiratory tech case study or explore Propeller Health’s research.
All-in-One Telemedicine Kits
Telemedicine kits are collapsing the distance between patients and providers, packing clinic-grade diagnostics into portable, AI-driven systems. These kits—equipped with digital stethoscopes, ECG monitors, and AI triage—are bridging gaps in rural care, disaster zones, and home health, ensuring no one is left undiagnosed due to geography.
How They Work:
A typical kit, like HealthCube Pro, includes:
- Digital Stethoscope: Captures heart and lung sounds, transmitting them via Bluetooth for remote specialist review.
- 12-Lead ECG: AI flags arrhythmias or ST-segment elevations in real time.
- AI Triage Software: Prioritizes cases based on urgency (e.g., chest pain over rashes), cutting wait times by 50% in trials.
Impact on Underserved Communities:
In Amazon Basin clinics, community health workers using kits diagnosed 80% of tuberculosis and Chagas disease cases onsite, eliminating multi-day treks to urban hospitals. Similarly, post-earthquake Nepal saw ER overcrowding drop by 45% as kits enabled (triage) in tent camps.
Regulatory & Clinical Validation:
- FDA-cleared kits like TytoCare now integrate with Epic and Cerner, letting PCPs bill for virtual exams.
- A 2024 NEJM study linked AI triage to a 30% reduction in missed heart failure diagnoses in home health settings.
Next-gen kits add retinal cameras for diabetic retinopathy and low-cost ultrasound wands, guided by AI to capture diagnostically viable images.

Source: theacedamic.com
The Indian government introduced telemedicine guidelines to overcome the difficulties of enabling policy, regulatory framework, and medical liability. It has taken action to solve the issues with patient privacy and confidentiality, data storage, data correctness, data privacy, data security.
G. Jabarethina
Explore how telemedicine kits are closing care gaps in remote healthcare report or learn to implement them via WHO’s digital health toolkit.
Bonus: Healthcare Innovations Poised to Transform the Next Decade
While the top 10 devices dominate 2025’s spotlight, these emerging innovations hint at healthcare’s next frontier—where AI, wearables, and precision diagnostics merge to prevent rather than treat.
1. AI-Driven Imaging Revolution
Startups like Cleerly are redefining cardiac care with AI that analyzes coronary CT scans to quantify plaque composition. Unlike traditional methods, Cleerly’s algorithms predict rupture risks in lesions, guiding preemptive stenting.
Meanwhile, Qure.ai automates tuberculosis detection in chest X-rays with 98% sensitivity, slashing diagnostic delays in low-resource regions. A 2024 Gates Foundation trial linked Qure.ai to a 40% drop in TB mortality across Sub-Saharan Africa.
2. Wearables That Predict & Prevent
Wearables like Savemom are transforming maternal care by predicting and preventing complications. They continuously monitor vital signs, detecting deviations that could indicate risks like pre-eclampsia or premature labor.
Early warnings enable proactive measures, leading to healthier pregnancies and safer deliveries.
3. Cardiometabolic Diagnostics 2.0
RenalytixAI’s KidneyIntelX platform spots early-stage kidney disease via biomarkers and EHR data, identifying at-risk patients 5 years before symptoms. FDA-approved and validated in a 10,000-patient NHS study, it cut dialysis admissions by 22% in year one.
Startups like Eko Health are next, using AI stethoscopes to detect valvular heart disease during routine physicals.
Bioengineered skin grafts are transforming wound healing. These grafts use lab-grown human cells to regenerate tissue. They help burn victims and chronic wound patients heal faster. Traditional skin grafts have rejection risks, but these integrate naturally. This innovation improves outcomes and reduces scarring significantly.
Ivan Rodimushkin, Founder, CEO, XS Supply
shifting from reactive to proactive care. AI isn’t just aiding clinicians—it’s becoming a co-pilot in prevention, while wearables evolve into daily health guardians.
Dive deeper into AI’s role in future diagnostics or explore GOQii’s preventive models.
Conclusion
In 2025, medical devices are undergoing a transformative shift, revolutionizing diagnostics, treatment, and patient autonomy. Key innovations include AI-powered tools like surgical assistants and diagnostic platforms, personalized care through nanotechnology and 3D bioprinting, and remote empowerment via telemedicine kits.
Neurotech breakthroughs, such as brain-computer interfaces and smart prosthetics, are also restoring agency to individuals with disabilities. Looking ahead, AI is expected to evolve from an assistant to a collaborator, tackling complex conditions like dementia.
However, challenges remain, including regulatory frameworks, cost, data security, and ensuring equitable access to these innovations globally.
FAQs
How Do These Devices Enhance Patient Outcomes?
These innovative devices offer more accurate diagnoses, personalized treatments, and improved monitoring, leading to better overall patient care and recovery.
Are There Clinical Trials Supporting The Effectiveness of These Devices?
Yes, each device has undergone rigorous testing and clinical trials to validate its effectiveness and safety before being introduced to the market.
How Accessible Will These Technologies Be?
While some devices are designed for hospital use, others like xKidney and Smart Glucose Monitors are made for home use, increasing accessibility. However, cost and insurance coverage may vary.
What Role Does AI Play in these Medical Devices?
AI is crucial in many of these devices, enabling features like predictive analytics, personalized treatment recommendations, and automated anomaly detection.
How Do These Devices Integrate with Existing Hospital Systems?
Most of these devices are designed with interoperability in mind, allowing for seamless integration with Electronic Health Records (EHR) and other hospital systems.